
Contents:
Breathing, Thinking, Functioning (BFT)
The BFT Model is a tool to help Healthcare Professionals understand, assess and manage chronic breathlessness
Reference: Cambridge BTF: www.btf.phpc.cam.ac.uk
Breathing
Dysfunctional breathing patterns are common. Breathless patients experience a sense of ‘needing more air’ and so increase their respiratory rate, using predominantly the upper chest and accessory muscles, further increasing the work of breathing and intensifying breathlessness.
- Breathing techniques
- Handheld fan
- Airway clearance techniques
- Inspiratory muscle training
- Chest wall vibration
- Non-invasive ventilation
“It is natural to think when you are feeling breathless that you need more air in. In fact this isn’t the case -we know that there is plenty of air in your lungs. Try instead to lengthen your out breath, which can make your breathing more efficient and create space for your next breath.”
Thinking
Breathlessness can cause fear and anxiety which in turn can worsen the perception of breathlessness. This can easily lead to panic attacks which in turn can increase the respiratory rate and cause muscle tension, further increasing the work of breathing and the feeling of breathlessness.
- Cognitive behavioural therapy (CBT)
- Relaxation techniques
- Mindfulness
- Acupuncture
“Some people say that they’re terrified that they are going to die gasping for breath. Although this is an understandable feeling, this almost never happens” (Then give a relevant explanation for a particular patient, for example “At that time, waste gases tend to build up in the blood, making people feel calm and sleepy.)”
Functioning
Breathlessness leads to inactivity which leads to muscle deconditioning which increases the demand on the respiratory system, and worsens breathlessness further.
- Pulmonary rehabilitation
- Cardiac Pulmonary rehabilitation
- Activity promotion
- Walking aids
- Pacing
- Neuromuscular electrical stimulation
- Hospice self-management programme if patient end stage/palliative or pulmonary rehab unsuitable
“Choosing to make yourself moderately breathless by being active is not harming you. In fact it builds up fitness in your muscles again and can improve your breathing and general health over weeks and months.”
Non-pharmacological management should be considered for all patients with breathlessness
- Explanation of cause/reassurance/calm manner
- Simple measures such as; keep room cool; use of a fan; open window; relaxation & breathing techniques
- Posture – ideally upright & leaning forward if possible
- Nutritional advice
- Treat depression/anxiety if present
- Encourage social interaction (peer group support; Breathe Easy group; breathlessness management in hospice day unit where appropriate)
- Lifestyle advice and appropriate signposting/referral
- Consider smoking cessation referral & management
- Consider referral to Physiotherapist/Occupational therapists
- Diaphragmatic breathing technique; pursed lip breathing technique; visualisation techniques to encourage longer expiratory phase
- Relaxation training
- Energy conservation/pacing training/equipment adaptations in activities of daily living & lifestyle expectations
- Strategies to manage other physical symptoms, psychological, social & spiritual needs of patient & family
- Use of Complementary therapy to aid relaxation techniques; such as Palliative Complementary therapy services at e.g. hospices
- Hold the fan about 6 inches (15cm) from your face or the distance you find most helpful
- Aim the cool air at your cheeks, nose and mouth.
- Either hold the fan still or move it around slightly, whatever you find most helpful.
From Bringing Breathlessness into View – a guide to living well with breathlessness: hyms.ac.uk
Watch “Using a handheld fan to reduce breathlessness” on YouTube
“Would you be surprised if the patient died within the next year ?”
– If NO then consider the following…
- Advance Care Planning
- Gold Standards Framework
- ReSPECT Forms
- Refer to palliative care team
“Breathing should be through the nose, using the diaphragm and done slowly. “Nose, low and slow”
- Breath in
- Breath out
- Breath in
- Breath out
Try to aim for breathing in for 2-3 seconds as you follow along the short edge of the rectangle and out for 4-5 seconds as you follow along the long edge of the rectangle. Try to develop a rhythm with your breathing. Do not hold your breath, but aim for a relaxed transition between breathing in and out.
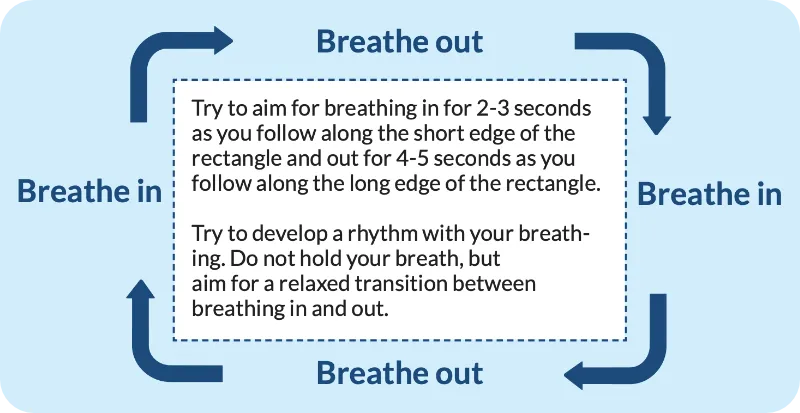
For more information: physiotherapyforbpd.org.uk
Grade 1
Are you ever troubled by breathlessness except on strenuous exertions?
Grade 2
Are you short of breath when hurrying on the level or walking up a slight hill?
Grade 3
Do you have to walk slower then most people on the level? Do you have to stop after a mile or so (or after 1/4 hour) on the level at your own pace?
Grade 4
Do you have to stop for breath walking about 100 yards (or after a few minutes) on the level?
Grade 5
Are you too breathless to leave the house, or breathless after undressing?
Disclaimer
These Guidelines are intended for use by healthcare professionals and the expectation is that they will use clinical judgement, medical, and nursing knowledge in applying the general principles and recommendations contained within. They are not meant to replace the many available texts on the subject of palliative care.
Some of the management strategies describe the use of drugs outside their licensed indications. They are, however, established and accepted good practice. Please refer to the current BNF for further guidance.
Whilst SPAGG takes every care to compile accurate information , we cannot guarantee its correctness and completeness, and it is subject to change. We do not accept responsibility for any loss, damage or expense resulting from the use of this information.
