

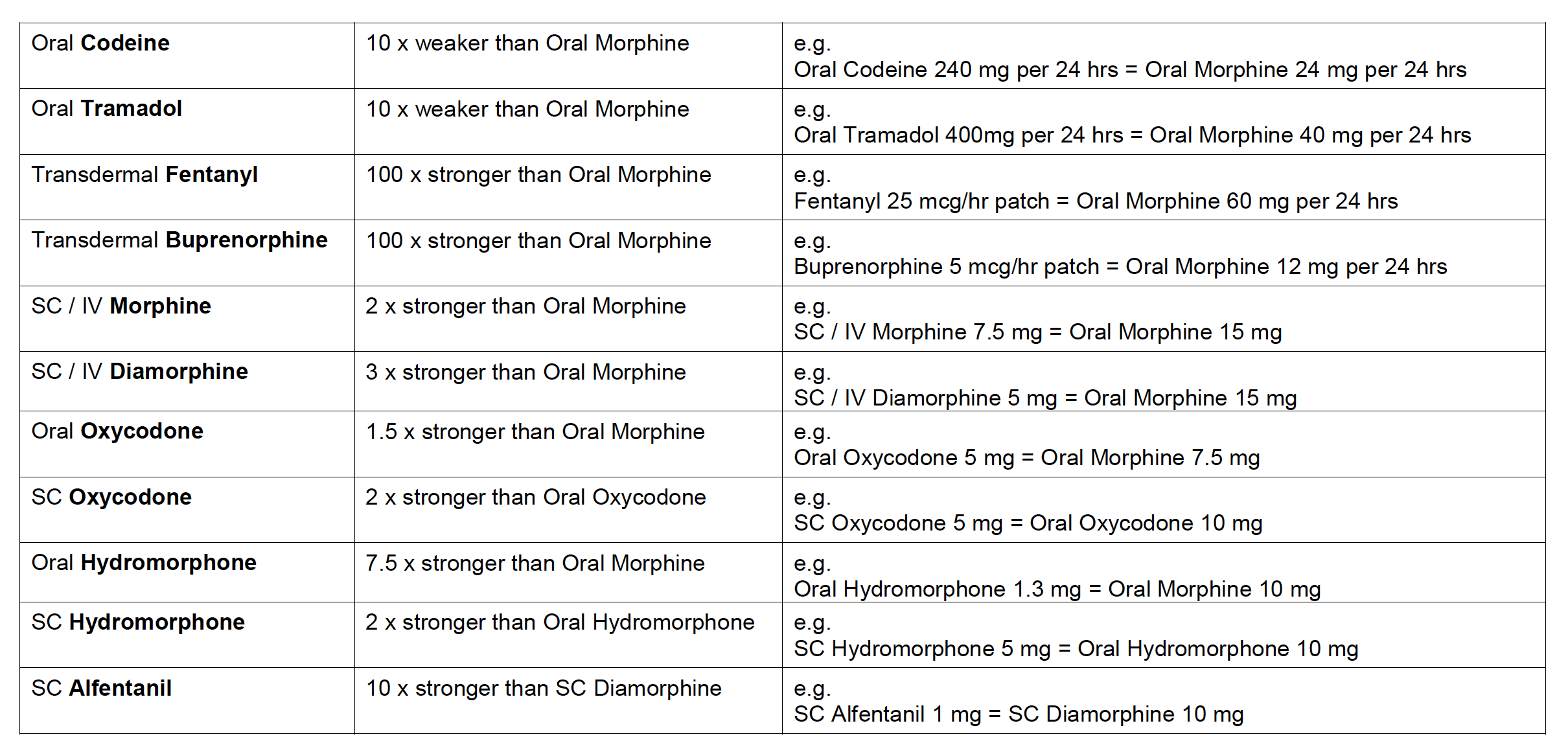
Alternative strong opioids to morphine may be used to try to improve compliance or the side-effect profile for patients.
Their use must be individually tailored and the following tables should be used as guidance only together with information in the following text.
Specialist palliative care advice is usually needed when changing from one strong opioid to another. Usually convert to a slightly lower equivalent dose and provide appropriate PRN breakthrough analgesia for titration.
Palliative Care: opioid equianalgesic dose conversions
- These are approximate dose conversions, caution is always necessary but particularly when converting at high doses and when there has been a recent rapid escalation of initial opioid; individual titration is necessary in order to optimise pain control after opioid switching
- A switch to methadone should only be undertaken by practitioners experienced in its use; equianalgesic dose conversions cannot be recommended for this opioid because of the wide inter-individual variation in pharmacokinetics of methadone
- Conversion ratios between oxycodone and other opioids in particular have some regional variation in clinical practice which is reflected in the table and text below. The table assumes an oxycodone to morphine ratio of 1:1.5. However, due to conversion ranges of 1.5-2 being reported in evidence many practitioners may often use an oxycodone to morphine ratio of 1:2 and it is critical that local practice is clarified
- Using a morphine: oxycodone 2:1 ratio creates a large variation in end conversion calculation to other opioids such as alfentanil, compared to using a morphine: oxycodone 1.5:1 ratio. Although in practice this rarely presents difficulties or causes of toxicity, caution may be required in deciding the most appropriate dose in this situation
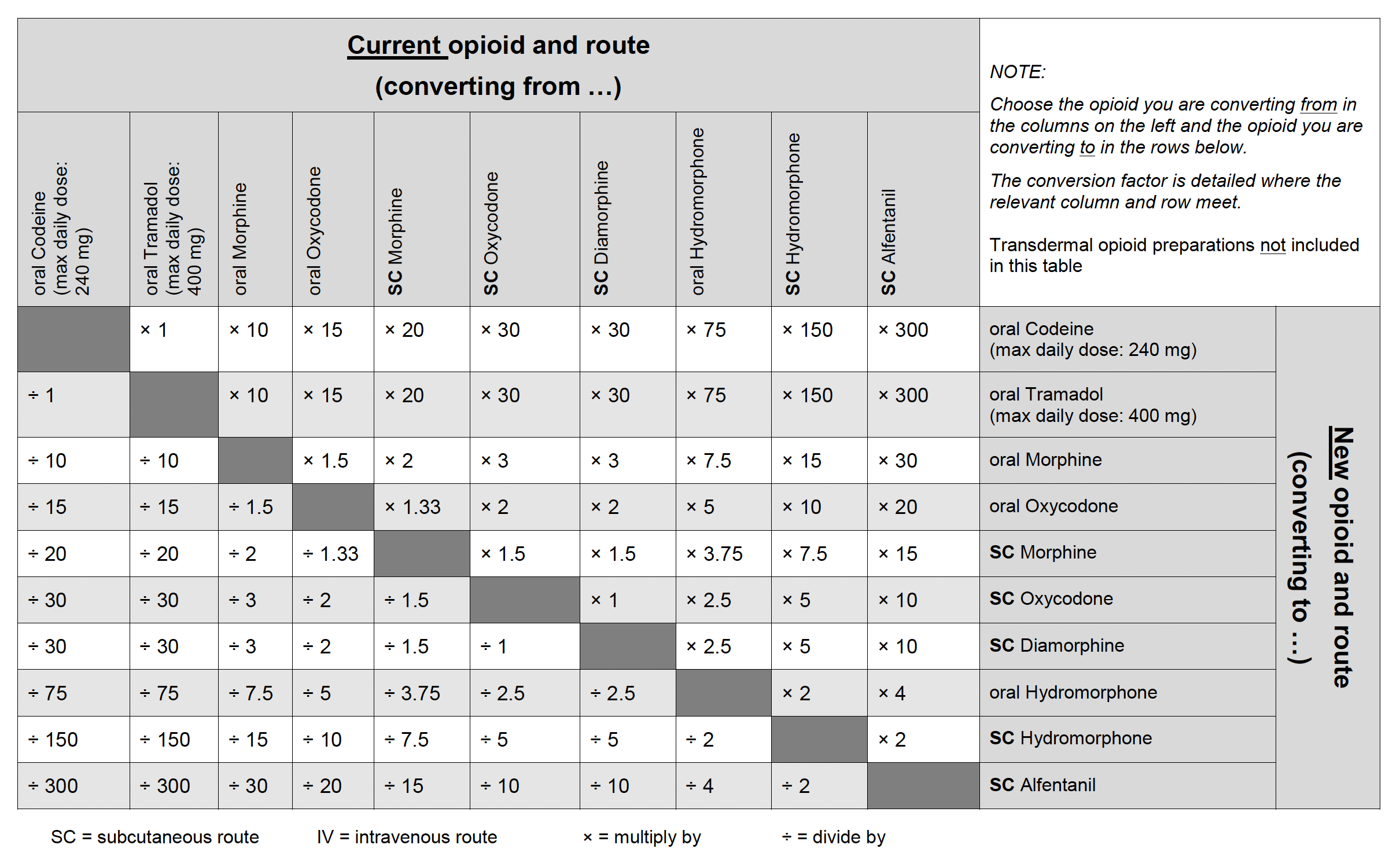
Opioid Conversion Chart
Quick Check Table
Converting between morphine and diamorphine
Approximate equivalent doses of oral morphine and subcutaneous morphine and subcutaneous diamorphine:
3mg oral morphine = 1.5mg SC morphine = 1mg SC diamorphine
These conversion ratios apply to PRN. and regular dosing.
Example 1
60mg morphine slow release tablet BD PO
=total daily dose oral morphine 120mg PO
=60mg SC morphine/24 hrs
=40mg SC diamorphine/24 hrs
Example 2
30mg Oramorph PO PRN
=15mg SC morphine PRN
=10mg SC diamorphine PRN
Converting between morphine and transdermal patches
See Section: Transdermal opioids
1mg SC diamorphine = 3mg oral morphine = 1.5mg SC morphine
Diamorphine was traditionally used as the first line injectable strong opioid as it is more water soluble than morphine. Morphine sulfate injection is now used in many centres as the first line injectable strong opioid.
Diamorphine preparations:
Injection: 5mg, 10mg, 30mg, 100mg, 500mg in packs of 5 ampoules
10mg oral oxycodone = 5mg SC oxycodone
10mg oral oxycodone = 15mg–20mg oral morphine = 7.5mg–10mg SC morphine
• Oxycodone has good oral bioavailability
• Oxycodone is usually the second line alternative if morphine is not tolerated
• The example above illustrates the dose conversion when oxycodone is regarded as being 1.5 – 2 times more potent than oral morphine
Care should be taken to ensure clarity when prescribing immediate release capsules or modified release tablets, particularly in view of differing generic brands now on the market.
Oxycodone preparations:
Immediate release (OxyNorm®) capsules, for PRN use:
5mg (orange/beige), 10mg (white/beige), 20mg (pink/beige) (packs of 56)
Oral solution (OxyNorm®) : 1mg/ml (250ml)
Concentrated oral solution (OxyNorm®): 10mg/ml (120ml)
Modified release tablets (OxyContin®) for 12-hourly administration:
5mg–light blue, 10mg–white, 15mg–grey, 20mg–pink, 30mg – brown, 40mg–yellow, 60mg–red, 80mg–green, 120mg–purple (packs of 56)
Injection: 10mg/ml: 1ml, 2ml ampoules. 50mg/ml: 1ml ampoules
Targinact®: The opioid antagonist naloxone is added to counteract opioid induced constipation by blocking the action of oxycodone at opioid receptors locally in the gut. Seek advice from specialist palliative care before prescribing (see chapter: Constipation).
1.3mg oral hydromorphone = 0.6mg SC hydromorphone = 10mg oral morphine = 5mg SC morphine
An alternative if morphine is not tolerated because of adverse effects under specialist guidance. Immediate and modified release capsules may be opened and sprinkled onto food.
Hydromorphone preparations (Palladone®):
Immediate release capsules:
1.3mg (orange/clear), 2.6mg (red/ clear) for PRN use (packs of 56)
Modified release capsules:
2mg (yellow/clear), 4mg (pale blue/ clear), 8mg (pink/clear), 16mg (brown/clear), 24mg (dark blue/ clear) for 12-hourly administration
Seek specialist palliative care advice.
1mg SC alfentanil = 10mg SC diamorphine = 30mg oral morphine = 15mg SC morphine
Suitable parenteral opioid for use in advanced renal disease under specialist guidance. Alfentanil has a short duration of action which limits its use for breakthrough analgesia.
Note very different dose conversions than fentanyl (see below for more info).
N.B. Alfentanil and fentanyl are different drugs.
Alfentanil preparations:
Injection (Rapifen®) 500 microgram per ml, 2ml, 10ml ampoules
Intensive Care Injection 5mg per ml, 1ml ampoules to be diluted before use
Always seek specialist advice.
Seek specialist palliative care advice.
150 micrograms SC fentanyl = 10 mg SC diamorphine =morphine 30 mg oral = 15 mg SC morphine
Suitable parenteral opioid for use in advanced renal disease under specialist guidance.
Also available as a transdermal patch see section: Transdermal fentanyl and as immediate release preparations (buccal, intranasal, sublingual and submucosal formulations) for incident pain see section: Transmucosal Fentanyl preparations.
Note very different dose conversions than alfentanil (see above for more information).
N.B. Alfentanil and fentanyl are different drugs.
Be aware that when prescribing a syringe driver/pump for fentanyl that the dose is micrograms per 24 hours whilst when administering a transdermal patch the dose is micrograms per hour.
Fentanyl injectable preparations:
Injection (generic) 50 microgram per ml, 2ml and 10 ml ampoules fentanyl (Sublimaze®) 50 microgram per ml, 10 ml ampoules
A novel analgesic combining mu opioid properties and noradrenaline reuptake inhibition. This can be helpful for pain that is mixed and has an element of nerve/neuropathic pain associated with it. At the time of writing there is limited experience of this in palliative care.
Seek specialist palliative care advice.
50mg Tapentadol = 15-20mg oral morphine
Tapentadol preparations:
Immediate release (Palexia®):
Tablets, f/c, tapentadol (as hydrochloride) 50mg (white), 75mg (yellow)
Oral solution, tapentadol (as hydrochloride) 20mg/ml
Modified release (Palexia®SR):
Tablets, f/c, 50mg, 100mg, 150mg, 200mg, 250mg
Disclaimer
This Guide is intended for use by healthcare professionals and the expectation is that they will use clinical judgement, medical, and nursing knowledge in applying the general principles and recommendations contained within. They are not meant to replace the many available texts on the subject of palliative care.
Some of the management strategies describe the use of drugs outside their licensed indications. They are, however, established and accepted good practice. Please refer to the current BNF for further guidance.
While WMPCPS takes every care to compile accurate information , we cannot guarantee its correctness and completeness and it is subject to change. We do not accept responsibility for any loss, damage or expense resulting from the use of this information.